World Hepatitis Day
By Peter Searles
The 28th of July is World Hepatitis Day. It is an opportunity to raise awareness in our community and to work together towards the elimination of viral hepatitis.
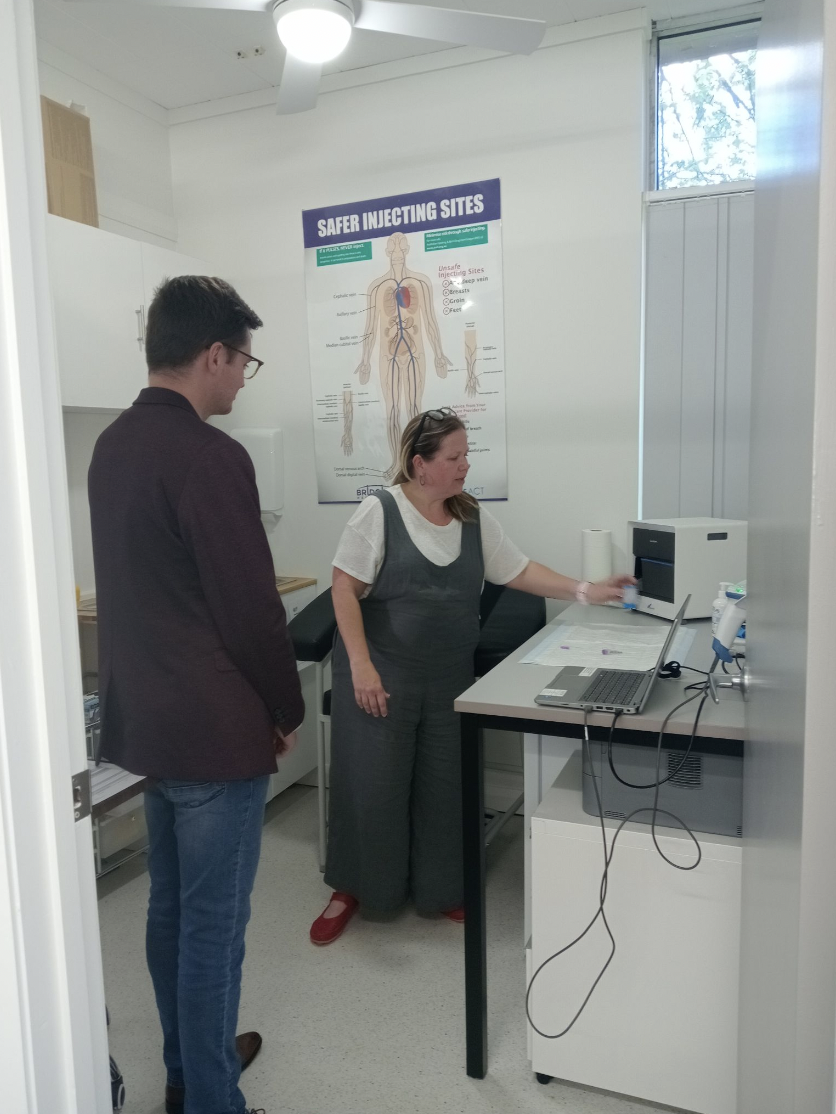
As a local community organisation, Hepatitis ACT aims to prevent transmission and reduce the impact on all people affected by viral hepatitis. I caught up with members of the team to get the facts about viral hepatitis and what we can do to keep our community safe and healthy.
WHAT IS HEPATITIS?
Hepatitis simply refers to inflammation of the liver. There are a variety of risk factors that may contribute to hepatitis such as viruses, lifestyle factors, medications, alcohol and auto-immune conditions. The work of Hepatitis ACT aims to address viral hepatitis, of which there are three types.
HEPATITIS A, B and C
Viral hepatitis includes hepatitis types A, B and C. There are different risk factors and prevalence in the community associated with each type of the virus.
Hepatitis A (Hep A) spreads most often through unclean food and drink. This is food or drink that has come into contact with infected poo. The main reasons this occurs are a lack of clean water and food not being cleaned correctly. You can also get hepatitis A through close physical contact with someone who has it and through oral or anal sex.
Several vaccine options are available to protect against Hep A in Australia. However, due to the low prevalence of the virus here, the vaccine is not recommended to all people. Information is available on the Hepatitis ACT website about preventing Hep A infection, as well as advice about when vaccination is recommended.
Hepatitis B (Hep B) is the most common form of viral hepatitis worldwide. It is a blood-borne virus, which means it can be transmitted via blood-to-blood contact with someone living with the virus. Once this contact occurs, Hep B travels to the liver where it multiplies by attaching to healthy liver cells. Hep B is also a Sexually Transmissible Infection (STI). Hep B infection can be acute (resolving after a short time) or chronic (continuing over a long period), with exposure occurring in infants and children being more likely to result in chronic infection.
While there is no cure, the Hep B vaccine is widely available and is generally administered to Australian newborns. In 2017, 96.3% of Australian children were vaccinated by the age of 2 years old. Due to the high vaccination rates, those living with Hep B in this country (roughly 200,385 people as of 2021) are largely people who have migrated here from overseas countries where vaccination rates are lower.
You can get hepatitis C (Hep C) if your blood comes into contact with infected blood. Some of the ways this can happen are:
sharing needles, syringes or other injecting equipment, including spoons
tattooing or body piercing with unsterile equipment
medical procedures with unsterile equipment
sharing toothbrushes, razors or nail files.
If you have hepatitis C when you are pregnant, there is about a 5% chance that you will pass on the virus to your baby. If you are pregnant and have hepatitis C, you should talk to your doctor. If you are thinking about getting pregnant and have hepatitis C, talk to your doctor about curing hepatitis C first.
Hep C is less likely to be transmitted sexually than Hep B as it is not carried in sexual fluids in sufficient quantities. However, when partaking in sexual activities where skin trauma can occur such as anal intercourse and rough sex, measures such as condoms, gloves and water-based lubricant should be used to minimise risk.
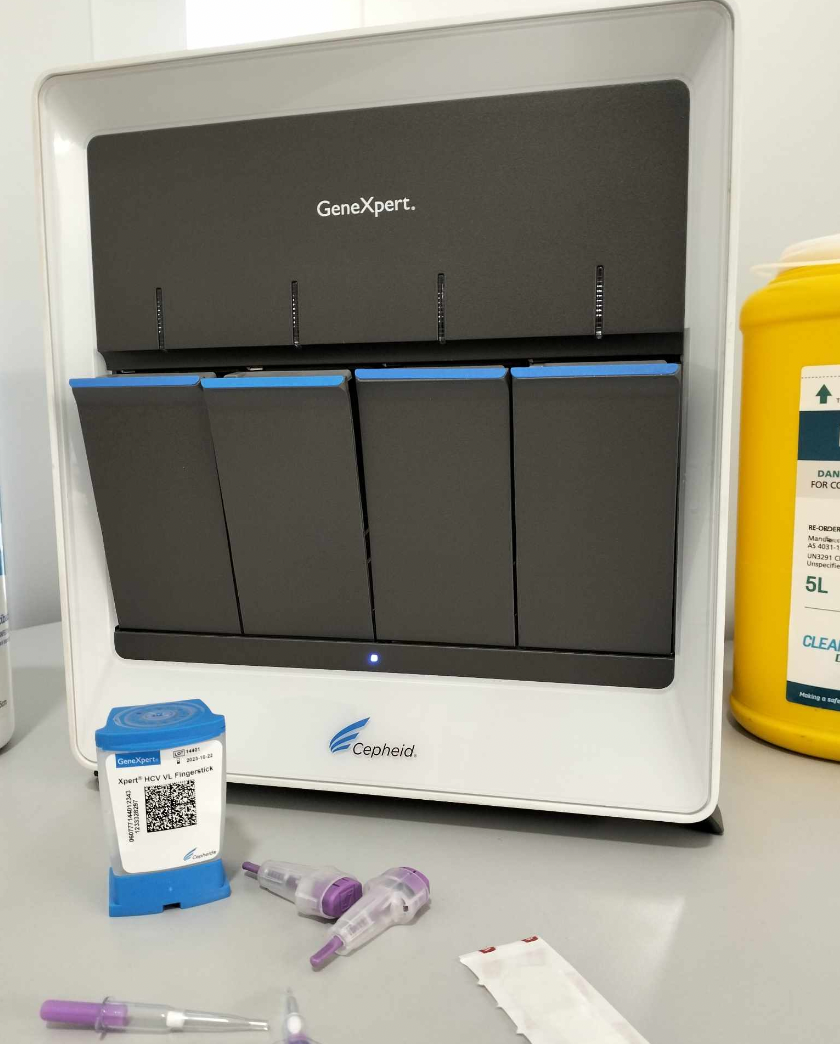
Hep C exposure in adults is far more likely to result in chronic infection than in cases of Hep B, but the good news is that an effective new treatment is available in the form of a tablet.
WHAT YOU SHOULD DO
If Hep B or Hep C infection is left untreated, it can cause liver damage and may lead to cirrhosis (scarring of the liver), liver cancer, or liver failure. So, it’s important to keep yourself safe through testing and vaccination.
Talk to your doctor about Hep B testing if you haven’t been vaccinated against the virus (or if you’re not sure). The Hep B test is not included in routine blood tests, but it is conducted for patients who are pregnant or those undergoing STI screening.
The Hep B vaccine is available from your GP or immunization provider. The vaccine is provided at no cost if you are part of the Medicare scheme.
If you would like assistance with Hep B vaccination, reach out to the national hepatitis infoline on 1800 437 222.
Hepatitis ACT also recommends hepatitis C testing during pregnancy and for those with specific risk factors.
You can find more information about hepatitis on the Hepatitis ACT website https://hepatitisact.com.au/, or call the national hepatitis infoline on 1800 437 222.